Introduction
Interoperability in healthcare is revolutionizing the way patient information is shared and utilized across systems and providers. This transformative force not only enhances patient safety and care but also streamlines workflows and improves operational efficiency.
In this article, we will explore the various benefits of interoperability in healthcare, including enhanced collaboration and communication, increased efficiency and productivity, better data accuracy and management, streamlined clinical workflows, and enhanced patient engagement and experience. Join us as we delve into the crucial role of interoperability in shaping the future of healthcare.
Improved Patient Safety
Interoperability in healthcare is a transformative force, enabling a seamless exchange of patient information across diverse systems and providers. This critical capability offers healthcare professionals immediate access to comprehensive and current patient data, fostering enhanced patient safety and care.
Through interoperability, healthcare providers gain an integrated perspective of a patient's medical history, encompassing medications, allergies, and prior treatments. This integration is crucial for minimizing errors and preventing adverse events.
A case in point is the introduction of MEG's Incident Reporting software in hospitals, which has revolutionized data analysis and incident management. Real-time dashboards provide immediate incident data to wards, allowing managers to oversee incidents, append comments, assign tasks, and refine processes in light of the insights gained.
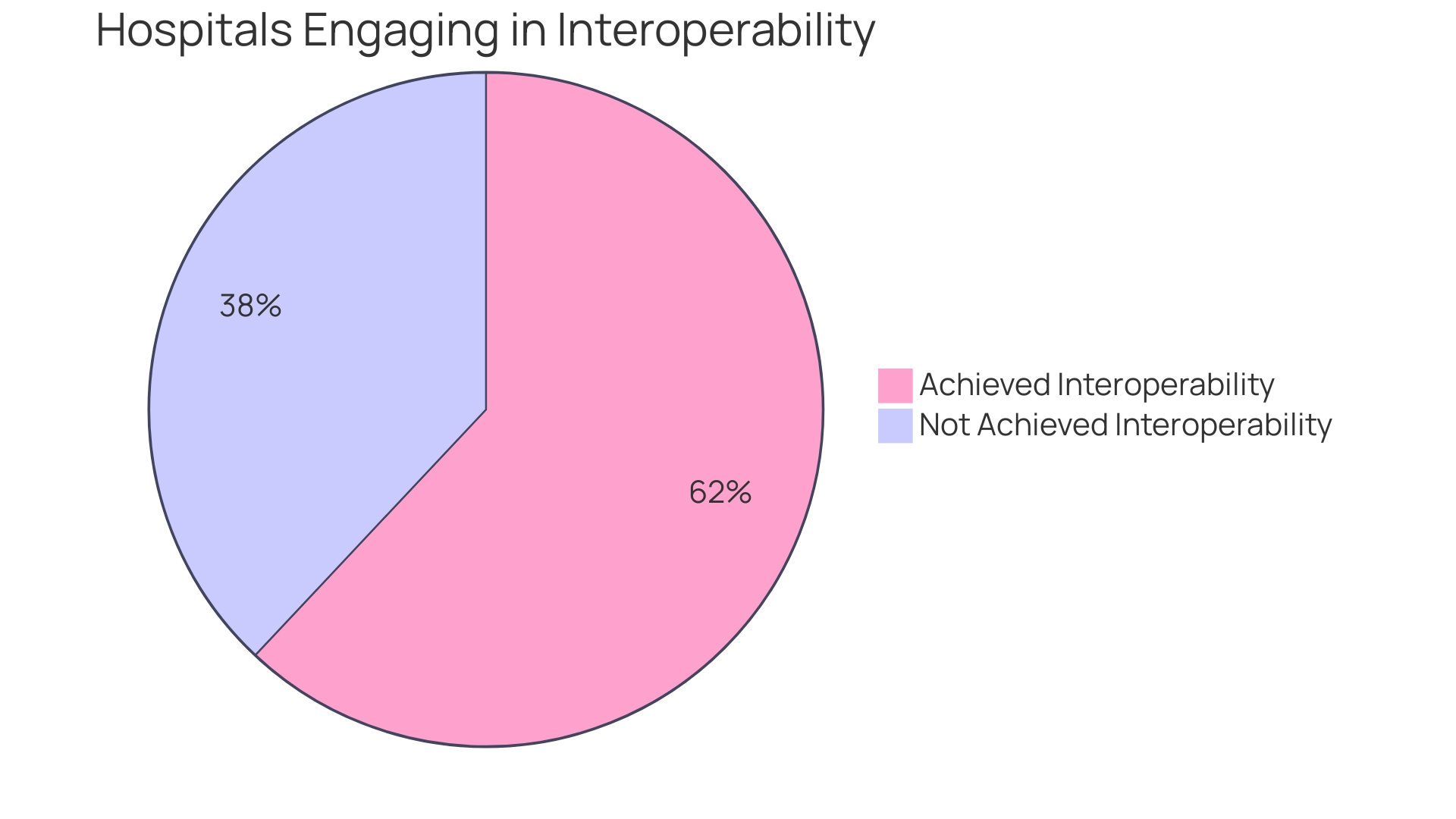
Such tools are not only instrumental in improving visibility and feedback across departments but also play a pivotal role in cultural transformation, redefining incident reporting as a valuable learning tool rather than a burdensome obligation. The journey towards healthcare interoperability has seen significant strides, with a report from The Office of the National Coordinator for Health Information Technology revealing a rise from 51% in 2017 to 62% in 2021 of hospitals engaging in electronically sharing health information.
Nevertheless, nearly 40% of hospitals have yet to achieve satisfactory interoperability. The Trusted Exchange Framework and Common Agreement (TEFCA) is expected to bolster connectivity, aiming to establish a universal baseline for interoperability nationwide. The promise of interoperability extends to efficiency by eliminating redundant tasks and setting the stage for successful automations and workflows, thereby dramatically reducing administrative burdens. It also enhances the patient experience by automating processes such as patient intake to avoid repetitive paperwork. For providers, interoperability translates into personalized care with faster diagnoses and reduced wait times, thanks to the seamless flow of accurate information. Ultimately, patients benefit from easy access to their complete medical history, leading to a more satisfactory healthcare experience.
Enhanced Collaboration and Communication
Interoperability in healthcare is not just a technical achievement; it's a vital component for enhancing patient care and operational efficiency. As healthcare technology evolves, the ability for diverse medical professionals to seamlessly share and utilize patient data in real time becomes crucial.
This interconnectedness allows for prompt decision-making and improved care coordination, which are essential in today's fast-paced medical environments. The significance of interoperability is evident in the recent push towards policies like the US Core Data for Interoperability (USCDI) and the Trusted Exchange Framework and Common Agreement (TEFCA), aiming for routine and valuable data exchange.
However, challenges remain, with one in three hospitals still not engaging in interoperable exchanges. The need for consistent and reliable electronic patient health information sharing is imperative to ensure it is useful when and where it's needed most. As we strive to close the gap, it's clear that interoperability not only contributes to better patient outcomes but also streamlines workflows, reduces manual tasks, and leads to a more positive experience for both healthcare professionals and patients. With a robust interoperable system in place, healthcare entities can achieve a comprehensive view of patient health, fostering transparency, and minimizing errors, ultimately paving the way for personalized and efficient patient care.

Increased Efficiency and Productivity
In the dynamic world of healthcare, the seamless exchange of electronic patient health information is not just a convenience; it's a lifeline for efficient operations and high-quality patient care. Interoperability in healthcare is the backbone that supports real-time access to critical data, allowing for prompt, informed decision-making.
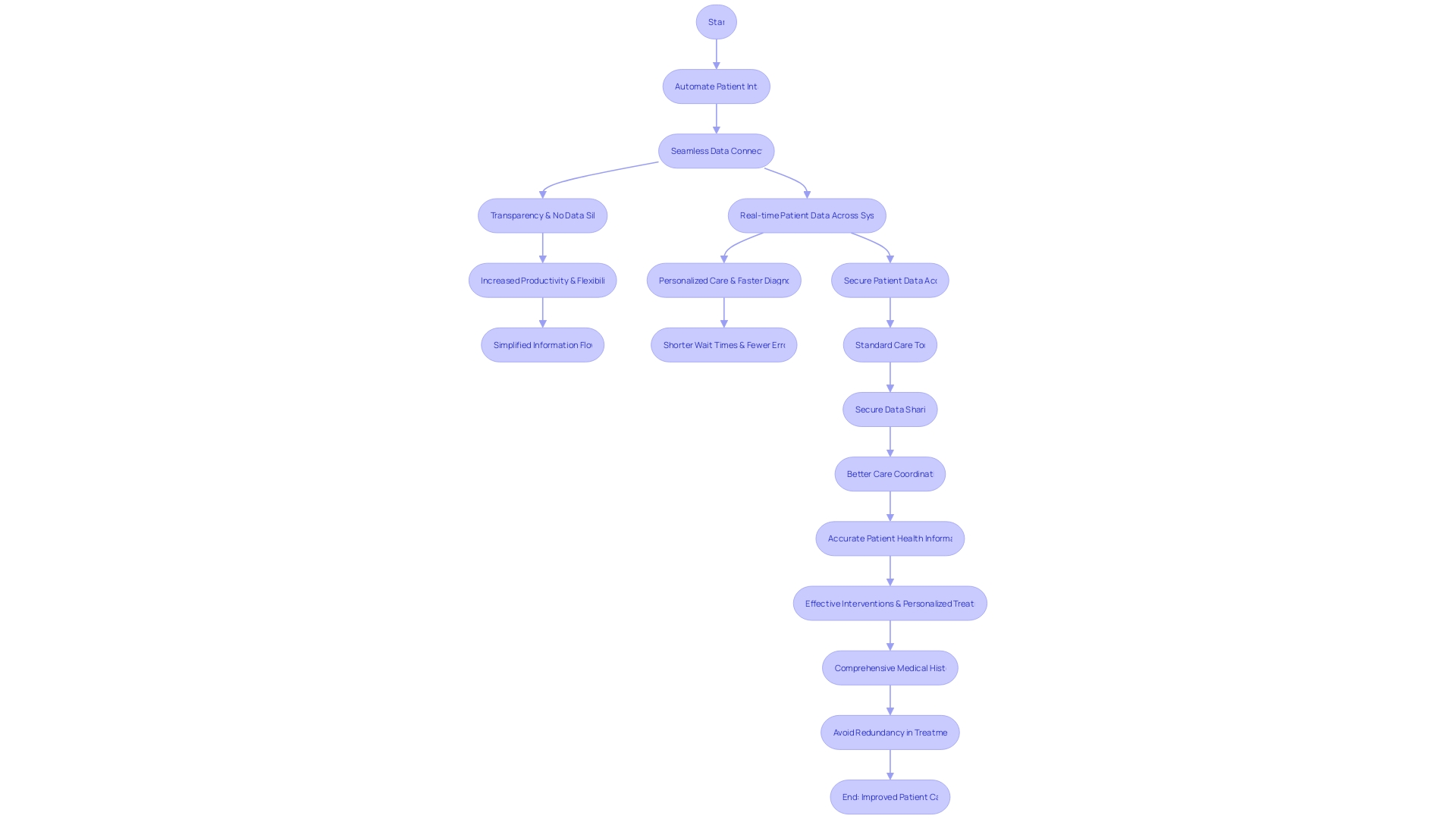
When healthcare providers can swiftly and securely access a patient's full medical history, the result is a dramatic increase in productivity, a reduction in administrative burdens, and the elimination of the all-too-common data silos. This interconnectedness translates to a streamlined workflow where tasks such as verifying insurance, scheduling appointments, and managing prescription refills become automated, releasing healthcare professionals to dedicate more time to direct patient care.
With interoperability, the patient experience is significantly enhanced. Automated patient intake processes minimize redundant paperwork, and the integration of care records from multiple providers offers a complete, 360-degree view of the patient's health.
This not only ensures transparency and accuracy but also fosters a more personalized approach to treatment, leading to faster diagnoses and shorter wait times. Despite these benefits, a report from The Office of the National Coordinator for Health Information Technology (ONC) reveals that in 2021, only 62% of hospitals were engaged in essential interoperability practices, and a third of hospitals rarely or never participated in interoperable exchanges. Moreover, rural and small hospitals lag behind in adopting these practices. The Trusted Exchange Framework and Common Agreement (TEFCA) aims to address these gaps, striving for a future where high-value, routine interoperability is a standard across the healthcare spectrum. As the industry moves forward, the focus will be on measuring progress and ensuring information is not only exchanged but also actionable at the point of care.
Better Data Accuracy and Management
The healthcare industry is undergoing a transformative shift towards seamless data exchange, and interoperability is at the heart of this evolution. By fostering the reliable sharing of electronic patient health information, interoperability enhances data accuracy and management, enabling healthcare providers to offer superior patient care.
The integration of systems permits consistent, real-time updates to patient records, which is crucial for informed decision-making and continuity of care. In the United States, initiatives such as the US Core Data for Interoperability (USCDI) and the Trusted Exchange Framework and Common Agreement (TEFCA) are paving the way for standardized data sharing.
These efforts are aligned with the goals of the Centers for Disease Control and Prevention (CDC) and the Centers for Medicare & Medicaid Services (CMS), which focus on the modernization of data and the delivery of value-based care. Statistics underscore the importance of interoperability: hospitals with routine interoperability are 92% more likely to have necessary clinical information available at the point of care.
Yet, a disparity exists, as only one in three hospitals report frequent interoperable exchange, and many physicians find it challenging to access and utilize external clinical information. Furthermore, the integration of patient health information into EHRs has seen a 40% growth since 2017, demonstrating a clear trend towards better data management.
The benefits are manifold, including higher efficiency, reduced administrative burdens, and a better experience for patients and healthcare staff alike. Tools developed by companies like the King of Prussia, PA-based subsidiary of Universal Health Services optimize EHRs, enhancing usability, safety, and satisfaction. Interoperability is not just a technological advancement but a patient-centric approach that ensures accurate, accessible, and actionable health information, which is vital for personalized care, faster diagnoses, and fewer errors. As healthcare continues to advance, the need for protected patient data access and the ability to share data cohesively becomes ever more critical. Monitoring the progress of interoperable exchange across all providers will remain essential in achieving real gains in patient outcomes and healthcare efficiency.
Streamlined Clinical Workflows
In the rapidly evolving healthcare landscape, interoperability emerges as a lynchpin for enhancing clinical workflows. By allowing seamless integration across diverse healthcare systems and applications, interoperability facilitates direct access to patient information within existing systems.
This integration circumvents the need for manual data entry or toggling among multiple platforms, thereby bolstering efficiency and reducing the administrative load. Clinicians are empowered to dedicate their efforts to patient care, thanks to the reduced friction in accessing critical patient data.
Moreover, interoperability paves the way for embedding decision support tools and clinical guidelines directly into care processes, thereby promoting standardized and effective treatment protocols. The transformative impact of interoperability is evidenced by recent data, which indicates that hospitals with routine interoperability are 92% more likely to have crucial clinical information accessible from external sources at the point of care.
The significance of this is twofold: it ensures continuity of care while sealing information gaps, resulting in enhanced patient outcomes. Despite these strides, challenges persist, with one in three hospitals reporting infrequent or non-existent interoperable exchanges. Furthermore, only a minority of physicians are fully engaged across all interoperability domains. Nonetheless, the push towards policies such as the Trusted Exchange Framework and Common Agreement (TEFCA) aims to standardize data sharing, which is fundamental for national health. The journey towards interoperability, while fraught with obstacles like fragmented systems and inconsistent standards, remains a critical endeavor for the healthcare industry, with the promise of a more integrated, efficient, and patient-centric healthcare system on the horizon.
Enhanced Patient Engagement and Experience
The transformative power of interoperability in healthcare cannot be overstated. Consider Sun Life Health, which serves a diverse patient base of over 48,000 individuals.
By integrating healow Insights into their operations, they were able to proactively address care gaps, streamline IT processes, and enhance planning for patient visits. This strategic move not only increased annual wellness visits but also led to a substantial revenue boost.
Similarly, Summer Health's collaboration with OpenAI and the implementation of GPT-4 for generating medical visit notes exemplifies efficiency gains. Pediatricians saw a fivefold reduction in administrative tasks, from ten minutes per visit note to two, freeing up valuable time for patient care.
These case studies underscore the critical role of interoperability in delivering personalized care and the positive impact on patient engagement and satisfaction. Statistics reinforce the significance of interoperability, with a notable rise from 28% to 43% in hospitals engaging in comprehensive interoperable exchange since 2018.
Yet, the journey isn't complete. Routine exchange is crucial for optimal care, and disparities persist, particularly in resource-limited facilities. Interoperability is not just a technological advancement; it's a catalyst for better healthcare. With real-time data access, healthcare providers can avoid unnecessary tests, reduce wait times, and eliminate errors, ultimately leading to a more satisfactory patient experience. In the words of an industry expert, 'The real-time access to patient health information allows providers to avoid miscommunications and provide more accurate patient health information.' This is the future of healthcare, where technology bridges gaps and fosters a seamless care continuum.
Conclusion
In conclusion, interoperability in healthcare is a transformative force that enhances patient safety, collaboration and communication, efficiency and productivity, data accuracy and management, streamlined clinical workflows, and patient engagement and experience. It enables seamless exchange of patient information across systems and providers, providing healthcare professionals with comprehensive and current patient data for informed decision-making.
Interoperability eliminates redundant tasks, automates processes, and reduces administrative burdens, resulting in improved operational efficiency. It also ensures better data accuracy and management by facilitating real-time updates to patient records.
Streamlined clinical workflows are achieved through direct access to patient information within existing systems, reducing the need for manual data entry. Moreover, interoperability enhances patient engagement and experience by delivering personalized care, faster diagnoses, shorter wait times, and easy access to complete medical history. As the healthcare industry continues to evolve, the focus remains on achieving universal interoperability to drive better patient outcomes and a more efficient healthcare system.





